 Overview
OverviewA Hammer toes is a misshapen second, third, or fourth toe. The toe bends up at the middle joint. The toe becomes a hammertoe because a muscle in the toe isn?t working properly or is too weak, increasing pressure on the tendons and the toe joints. Muscles normally work in twos to bend and straighten toes. If the toe stays bent too long, a hammertoe develops. Ill-fitting shoes, arthritis, heredity, even an injury, can cause the hammertoe to form. To add insult to injury, corns and calluses are common on top of hammertoes because the toe is rubbing against the shoe.
Causes
While ill-fitting shoes may contribute to a hammertoe, shoes don't actually cause it, Hammertoes occur by the pull and stretch of the tendon. One tendon gets a more mechanical advantage over the other and allows the deformity to occur. Not surprisingly, wearing shoes that are too tight can make a hammertoe worse. If you're fond of narrow, pointy-toed shoes or high-heeled pumps, keep in mind you're squeezing those toes and tendons, which may aggravate hammertoes.
 Symptoms
SymptomsSome people never have troubles with hammer toes. In fact, some people don't even know they have them. They can become uncomfortable, especially while wearing shoes. Many people who develop symptoms with hammer toes will develop corns, blisters and pain on the top of the toe, where it rubs against the shoe or between the toes, where it rubs against the adjacent toe. You can also develop calluses on the balls of the feet, as well as cramping, aching and an overall fatigue in the foot and leg.
Diagnosis
Hammer toes may be easily detected through observation. The malformation of the person's toes hammertoes begin as mild distortions, yet may worsen over time - especially if the factors causing the hammer toes are not eased or removed. If the condition is paid attention to early enough, the person's toes may not be permanently damaged and may be treated without having to receive surgical intervention. If the person's toes remain untreated for too long, however the muscles within the toes might stiffen even more and will require invasive procedures to correct the deformity.
Non Surgical Treatment
Your doctor will decide what type of hammertoe you have and rule out other medical conditions. Treatment may range from more appropriate footgear to periodic trimming and padding of the corn. Cortisone injections may be indicated if a bursitis is present. Antibiotics may be utilized in the presence of infection. Removable accommodative pads may be made for you.
Surgical Treatment
Probably the most frequent procedure performed is one called a Post or an Arthroplasty. In this case a small piece of bone is removed from the joint to straighten the toe. The toe is shortened somewhat, but there is still motion within the toe post-operatively. In other cases, an Arthrodesis is performed. This involves fusing the abnormally-contracted joint. The Taylor procedure fuses only the first joint in the toe, whereas the Lambrinudi procedure fuses both joints within the toe. Toes which have had these procedures are usually perfectly straight, but they take longer to heal and don't bend afterwards. A Hibbs procedure is a transfer of the toe's long extensor tendon to the top of the metatarsal bone. The idea of this procedure is to remove the deforming cause of the hammertoes (in this case, extensor substitution), but to preserve the tendon's function in dorsifexing the foot by reattaching it to the metatarsals. Fortunately, the Gotch (or Gotch and Kreuz) procedure--the removal of the base of the toe where it attaches to the foot, is done less frequently than in years past. The problem with this procedure is that it doesn't address the problem at the level of the deformity, and it causes the toe to become destabilized, often resulting in a toe that has contracted up and back onto the top of the foot. You can even have an Implant Arthroplasty procedure, where a small, false joint is inserted into place. There are several other procedures, as well.
 When your big toe is angled towards the second toe, the deformity is called a bunion (hallux valgus). This causes a bump on the side at the base of the big toe. In addition there is often thickening of the skin and tissues next to the affected joint. The thickened skin and tissues may become inflamed, swollen and painful. Sometimes a fluid-filled sac (bursa) develops over the joint.
When your big toe is angled towards the second toe, the deformity is called a bunion (hallux valgus). This causes a bump on the side at the base of the big toe. In addition there is often thickening of the skin and tissues next to the affected joint. The thickened skin and tissues may become inflamed, swollen and painful. Sometimes a fluid-filled sac (bursa) develops over the joint.


 The Achilles' tendon is located in the leg just behind and above the heel. As the connection between the heel and calf muscle, its function is to allow the bending of the foot downwards. Generally if there is a tear to the Achilles' tendon it will be known as a rupture. This can be a partial tear or a complete tear, although partial tears are much rarer.
The Achilles' tendon is located in the leg just behind and above the heel. As the connection between the heel and calf muscle, its function is to allow the bending of the foot downwards. Generally if there is a tear to the Achilles' tendon it will be known as a rupture. This can be a partial tear or a complete tear, although partial tears are much rarer.
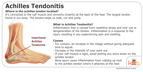 The Achilles tendon affects your ability to do everything from walking to playing competitive sports. When a patient overstretches his or her Achilles tendon, it can result in a full or partial tear in the tendon, also known as a rupture. In addition to causing a great deal of pain, ruptures can have a profoundly negative impact on your quality of life and prevent you from performing activities you once enjoyed. Because these injuries tend to worsen with time, it?s important to contact a board certified orthopedic surgeon for immediate attention after an Achilles tendon tear.
The Achilles tendon affects your ability to do everything from walking to playing competitive sports. When a patient overstretches his or her Achilles tendon, it can result in a full or partial tear in the tendon, also known as a rupture. In addition to causing a great deal of pain, ruptures can have a profoundly negative impact on your quality of life and prevent you from performing activities you once enjoyed. Because these injuries tend to worsen with time, it?s important to contact a board certified orthopedic surgeon for immediate attention after an Achilles tendon tear.


